ATLANTA – For years, researchers at the National Institutes of Health (NIH), the Centers for Disease Control and Prevention (CDC) and at pharmaceutical companies have tried unsuccessfully to create a successful gonorrhea vaccine. Clinical trials have been disappointing; potential vaccines have not generated an immune response. Researchers do know that the immune memory response does not last long in people who have been infected with gonorrhea, as they easily get re-infected.
Gonorrhea typically is treated with antibiotics, but Neisseria gonorrhoeae bacteria have become increasingly resistant to them, and drug options have dwindled. In 2006, the CDC had five recommended antibiotics for gonorrhea; now only one option remains for effective treatment in the United States, where there are 400,000 reported cases of gonorrhea each year.
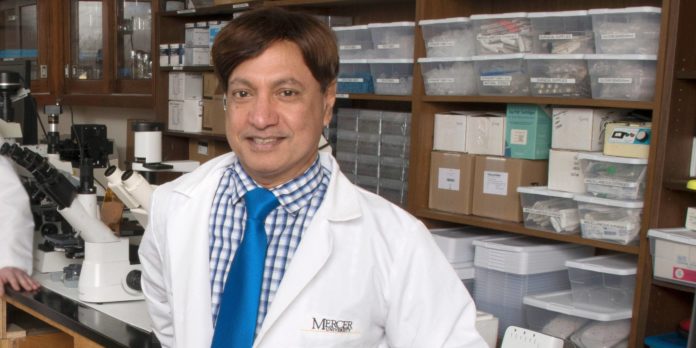
Now a “superbug” gonorrhea strain has emerged that is drug-resistant, making the need for a vaccine ever so more important. While a number of researchers are working on developing a vaccine, Mercer University’s pharmaceutical scientist Martin D’Souza has developed an innovative gonorrhea vaccine candidate that takes a novel approach.
Many of the failed vaccine attempts involve N. gonorrhoeae strains suspended in solution, but Dr. D’Souza’s potential vaccine is different. His vaccine candidate is dry. The bacteria strains are freeze-dried and then incorporated into microneedles made of sugar polymers. A microneedle patch is applied to the skin much like an adhesive bandage, with the microneedles dissolving in less than two minutes. The vaccine is released into the skin, where the microscopic particles are picked up by immune cells.
Since there’s no water in the final microneedle vaccine, this vaccine does not require refrigeration that current vaccines do. It can be kept at room temperature for years.
“Many vaccines are given by intra muscular or subcutaneous injection, but a significant portion is flushed out by the body,” said Dr. D’Souza, professor of pharmaceutical sciences and co-director of Mercer’s Center for Drug Deliver Research.
Dr. D’Souza’s research team conducted a preliminary study of this potential vaccine on mice infected with gonorrhea. All of the mice that received a one-time vaccine dose survived and generated a very strong antibody response to the vaccine.
He recently received a $464,658 grant over three years from the National Institute of Allergy and Infectious Diseases to support further studies to see if the vaccine provokes a long-term memory response.
Dr. D’Souza also has also designed a spray-dried particulate vaccine for ovarian cancer, which also was funded by the NIH. This vaccine is expected to enter Phase I trials in early 2019 and will be the first ovarian cancer vaccine to reach clinical trials. Dr. D’Souza is working with the Houston, Texas-based Kiromic Biopharma, which will oversee the trials at MD Anderson Cancer Center. Patients will take the vaccine by capsule.