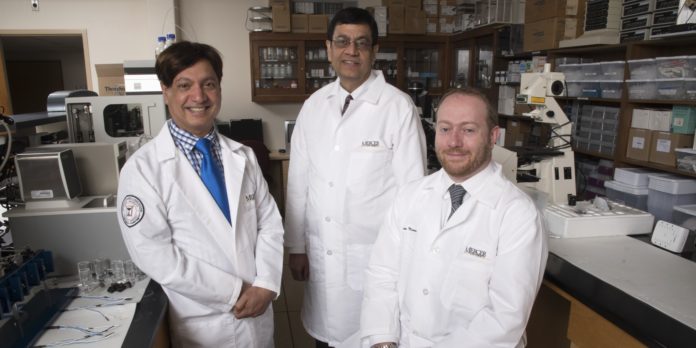
Three Mercer University researchers are working on new drug formulations that could more safely and effectively treat psychiatric and neurological disorders.
Through their company, DD Therapeutics, the researchers — Dr. Ajay Banga, Dr. Martin D’Souza and Dr. Kevin Murnane — hope to eventually commercialize products and bring them to market for the benefit of those suffering from brain disease.
“We want our research to reach out beyond our labs and make a difference in people’s lives,” said Dr. Murnane, assistant professor of pharmaceutical sciences in the College of Pharmacy.
Because of the brain’s complexity, brain disease has been notoriously hard to treat. Many medications bypass the brain altogether or can be unsafe to use. While many researchers have focused on discovering new brain systems to treat, such as newly discovered brain receptors or brain circuits, the DD Therapeutics team decided to go a different way and focus on drug formulation.
That is, they’re taking existing drugs and delivering them in a way that makes them safer and more effective to use.
They’re doing this in two ways: through transdermal delivery and nanotechnology.
Advantages of transdermal delivery
Transdermal delivery is when drugs are administered through the skin, such as through a patch.
DD Therapeutics’s lead product is a transdermal drug that could be used to treat attention-deficit/hyperactivity disorder (ADHD) or control weight through appetite suppression.
Using a patch to deliver the drug has many benefits over swallowing a pill, said Dr. Banga, professor of pharmaceutical sciences and an expert on transdermal delivery.
A patient may stick a patch to the skin for several days, rather than taking possibly multiple doses of pills per day. This increases patient compliance. In addition, when a drug is absorbed through the skin, it goes directly into the blood, bypassing the liver where many drugs are degraded, Dr. Banga said.
In terms of the patch for ADHD, patients may experience fewer unwanted side effects, Dr. Murnane said.
Many ADHD medications are stimulants and, while effective, may cause appetite loss and insomnia. Because of the time it takes the medication to enter the blood after swallowing a pill, patients may not be hungry at breakfast or unable to sleep at night, Dr. Murnane said.
But with a patch, the onset and offset of the drug is immediate, he said. That means patients could wait to apply the patch until they get to work or school and take off the patch before bed.
In addition, the patches can be made abuse deterrent, so the drug can’t be diverted and abused like pills, Dr. Murnane said.
“It doesn’t really change efficacy, but it makes it a much safer and more compliant product,” he said.
Nanoparticles help drugs enter the brain
DD Therapeutics also is using nanotechnology to treat some brain diseases with drugs that have trouble entering the brain through other delivery methods.
One of these drugs is oxytocin, a hormone that occurs naturally in the brain. Individuals with conditions like Parkinson’s disease and epilepsy are found to have less oxytocin, which is necessary for proper performance of certain brain functions, said Dr. D’Souza, professor of pharmaceutical sciences, who specializes in nanotechnology.
In his lab, Dr. D’Souza creates nanoparticles of oxytocin encapsulated in a biodegradable matrix that may be administered through the nose, similar to a nasal spray. This allows the drug to go directly to the brain, bypassing the rest of the body and the liver, where it may be degraded.
“In doing that, you can essentially deliver drugs very specifically to the brain area,” Dr. D’Souza said.
Both the transdermal and nanoparticle delivery systems have applications in a wide range of diseases that can be expanded down the road.
“Between Dr. Banga’s lab, my lab and Dr. Murnane’s expertise in the central nervous system, I think we cover a pretty broad spectrum of applications that can be used with these technologies,” Dr. D’Souza said.
A look to the future
DD Therapeutics formed in 2017 when the Georgia Research Alliance (GRA) awarded Phase 1 funding of $50,000 to the three Mercer researchers to assess the viability of the company.
Since then, it has received a $150,000 grant from the National Institutes of Health through the federal Small Business Technology Transfer program and an additional $100,000 grant from GRA. The Phase 2 GRA funding, awarded last year, is for continued research and development, as well as regulatory affairs.
DD Therapeutics has published numerous papers in peer-reviewed research journals and filed for several patents. The researchers are looking at starting clinical trials in the next three to five years, Dr. Murnane said.
Eventually, the hope is for DD Therapeutics to be a large pharmaceutical company that has gone through clinical trials and brought products to market, returning royalties to Mercer that can further advance research at the University.
GRA’s support has been invaluable, Dr. Murnane said, not only in terms of funding but also guidance and connections.
“They are a tremendous resource for us,” he said.
The headquarters for DD Therapeutics — the “DD” in the name stands for “drug delivery” — is in Atlanta Tech Village. Down the line, Dr. Murnane said he would like to see a facility potentially in Macon where Mercer students could have internship and employment opportunities.