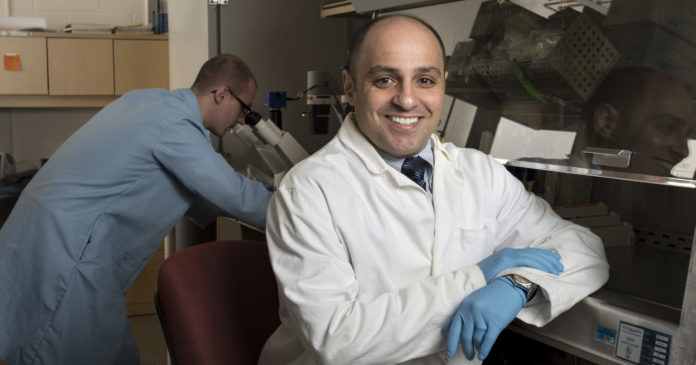
Dr. Nader Moniri, associate dean of research in the College of Pharmacy, received renewed funding from the National Institutes of Health to continue studying a key reason as to why common inhalation medications to treat asthma often become ineffective.
The grant renewal of $424,500, over three years, from the National Heart, Blood and Lung Institute will allow Dr. Moniri and his research team to continue examining how beta-2 receptor agonists, when inhaled for the fast rescue of asthma, stop working over time. His team believes tolerance to these drugs occurs due to oxidative stress in the lungs.
Asthma is a chronic inflammatory disease of the lungs characterized by airway obstruction and spasms of the muscles that line the airway. The gold standard treatment for asthma since the 1970s is an inhaler, containing a beta-2 adrenergic receptor agonist drug, like albuterol or formoterol, that relaxes the airways and reduces bronchospasms. Over time these inhaled drugs often become ineffective for patients.
The lungs contain reactive oxygen species, or ROS, which are natural byproducts of oxygen metabolism. While a certain level of ROS is normal, in asthma there is an overabundance of ROS, which contributes to constricting the muscles and exacerbating inflammation. The beta-2 agonists in inhalation medications relax the muscles in the airway by activating beta-2 receptors, however, over time—sometimes in just weeks or months—the medications stop working for patients.
ROS oxidizes the drug’s beta-2 receptors, and the Moniri research team. previously determined that while the beta-2 receptors need some levels of ROS oxidation to function, it now believes that over-oxidation of the beta-2 receptors by ROS in asthma continues to such a point that the agonist drugs become ineffective.
“With this new study, we will examine the role of over-oxidation of these receptors and how that contributes to the efficacy of these drugs over time,” Dr. Moniri said. “The hope is that we can identify drugs that don’t cause a high degree of this over-oxidation or couple these drugs with antioxidants or other approaches to help decrease the ROS and preserve their effectiveness in asthma.”
In a separate study, the Moniri research group previously identified an omega-3 fatty acid receptor, known as free-fatty acid receptor-4, or FFA4, that reduces inflammation. Drugs that activate the FFA4 in white blood cells also produced a significant reduction in ROS, which also may be viable treatments to decrease oxidation and reduce inflammation in asthma.
“Our end goal is understanding the mechanisms and pathways that are present in asthma to design drugs in the future that don’t activate the harmful pathways,” he said.
Dr. Moniri has been continually funded by the NIH since 2012, and this grant is the fourth he has received as principal investigator from NIH.
He is a professor of pharmaceutical sciences in the College and a professor of biomedical sciences in Mercer University School of Medicine. His research interests include signal transduction of G protein-coupled receptors and design and development of novel drugs that modulate the function of these receptors. His lab studies these receptors, including the beta-2 receptor and FFA4, in a variety of diseases including asthma, diabetes, inflammation, Parkinson’s Disease and cancer.